Irritable Bowel Syndrome (IBS) is a condition that affects millions of people worldwide, yet its root causes often remain misunderstood. While many assume IBS is purely genetic, research reveals a more complex picture. Through the Mind-Gut-Immunity Method, patients are learning how to address IBS at its core, achieving lasting relief by tackling the factors that activate inflammation and disrupt gut health.
This blog explores the root causes of IBS, focusing on actionable steps to manage the condition naturally and effectively.
The Genetics of IBS: Myths and Facts
A common misconception about IBS is that it’s entirely genetic. While genome-wide association studies (GWAS) have identified several dozen genes linked to IBS, these genes don’t act in isolation. Dr. Chanu Dasari explains, “You had the same genes when you were a child, but you weren’t sick back then. What changed?” The answer lies in epigenetics, the study of how environmental factors can turn genes on or off.
IBS-related genes often remain dormant until triggered by factors like:
- Chronic inflammation
- Poor diet
- Imbalance in gut microbes
The good news? These triggers can be controlled, allowing individuals to manage or even reverse their symptoms.
Inflammation: The Heart of IBS
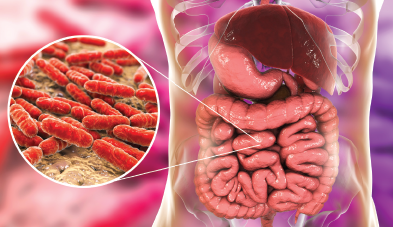
At its core, IBS is an inflammatory condition. Inflammation can stem from various sources, including poor digestion, microbial imbalances, and immune system dysregulation. Because 70-80% of the immune system resides in the gut, it’s no surprise that gut health plays a critical role in IBS.
Dr. Dasari emphasizes that inflammation in the gut can activate “bad genes,” exacerbating symptoms like bloating, diarrhea, constipation, and abdominal pain. Addressing this inflammation requires a holistic approach that targets both genetic and microbial factors.
The Five Epigenetic Root Causes of IBS
To effectively manage IBS, it’s essential to focus on five key environmental triggers. These “big five” factors influence how genes behave and directly impact gut health:
- Diet
- Diet is perhaps the most significant factor in managing IBS. A poor diet disrupts the gut microbiome, leading to inflammation and digestive issues.
- Focus on gut-friendly foods, such as high-fiber vegetables, fermented foods, and lean proteins, while avoiding processed foods, sugars, and known irritants.
- Digestion
- Troubled digestion often results from microbial imbalances, including Small Intestinal Bacterial Overgrowth (SIBO) or Candida overgrowth.
- Restoring balance involves promoting beneficial microbes and eliminating harmful ones. Probiotics and prebiotics can play a crucial role.
- Sleep
- Poor sleep disrupts the body’s natural healing processes and weakens the immune system. For IBS sufferers, quality sleep is essential for gut health.
- Prioritize a consistent sleep schedule, create a calming bedtime routine, and address any underlying sleep disorders like apnea.
- Stress
- Chronic stress triggers inflammation and worsens gut symptoms. While stress alone may not cause IBS, it exacerbates other triggers like poor eating habits and sleep deprivation.
- Incorporate stress-reducing activities such as meditation, yoga, or mindful breathing into your daily routine.
- Exercise
- A sedentary lifestyle contributes to inflammation and poor gut motility. Regular physical activity not only improves digestion but also reduces stress and supports overall well-being.
- Aim for at least 30 minutes of moderate exercise most days of the week, such as walking, swimming, or cycling.
The Role of the Gut Microbiome
One of the most fascinating discoveries in IBS research is the role of the gut microbiome. Only 1% of the genetic material in your body is human—the remaining 99% comes from the trillions of microbes living in your intestines. These microbes influence everything from digestion to immune response.
An imbalance in the microbiome, known as dysbiosis, can lead to:
- Increased inflammation
- Histamine dysfunction
- Bloating and gas
The Mind-Gut-Immunity Method focuses on promoting beneficial microbes while reducing harmful ones. By optimizing the microbiome, patients can achieve lasting relief from IBS symptoms.
Beyond the Big Five: Additional Triggers to Consider
While diet, digestion, sleep, stress, and exercise are the primary factors, other triggers can also contribute to IBS. These include:
- Smoking: Smoking increases inflammation and disrupts gut health.
- Dental Hygiene: Poor oral health can introduce harmful bacteria that affect the gut.
- Medication Side Effects: Certain medications can disrupt the microbiome or increase inflammation.
Addressing these secondary factors can further improve outcomes for IBS sufferers.
Taking Control of Your Health
IBS is a complex condition, but understanding its root causes provides a clear path to recovery. By focusing on diet, digestion, sleep, stress, and exercise, you can take control of your symptoms and improve your quality of life. The Mind-Gut-Immunity Method offers a comprehensive approach to managing IBS, emphasizing natural and sustainable solutions.
For personalized guidance and support, schedule a discovery call with Dr. Chanu Dasari at MGI Clinics. Our Case Studies page features stories of patients who have successfully managed their conditions through the Mind-Gut-Immunity Method.
Start Your Journey to Better Health Today
Discover the transformative power of the Mind-Gut-Immunity Method! Over the past decade, Dr. Dasari has helped countless clients reduce inflammation and find relief from autoimmune issues, often in just 3-6 weeks. Now, you can start your journey to better health with our free training. Click the link below, choose your condition, and learn how our proven approach can help you feel better fast.
About the Author
Dr. Chanu Dasari, a distinguished clinician with a career spanning renowned institutions like Vanderbilt University, Oxford University, and the University of California, has made significant contributions to medical research and practice. His work, published in top peer-reviewed scientific journals and adopted by the US Department of Health, highlights his commitment to advancing healthcare. Dr. Dasari is board-certified by the American Board of Medical Specialties and the American College of Surgeons, with a specialization in hernia repair, gallbladder removal, cysts, digestive disease, and cancer. As the founder of the Mind-Gut-Immunity Clinic, he draws from personal experience with autoimmune and digestive dysfunction to lead a team dedicated to patient-centered care using evidence-based protocols.