veryone who’s found those dry red blotches on their skin is familiar with the embarrassment, the irritation, and the frustration that comes with Psoriasis.
During our finals week, my study partner, Mick, broke out in a rash on his left tricep as well as his scalp. Furious to just get back to our exams, he just rubbed on some anti-itch cream and called it a day, stress rashes happen, right? After finals, the rashes went away, and things were fine until midterm exams came up in our last semester. This time the rash persisted for months until even after our graduation. The rash went from bad to worse, and was now burning, raised, and scaly. That whole time Mick stopped changing at the gym, or even wearing short-sleeved shirts at all, and he would become massively self-conscious during job interviews and even at work after that, and the constant scratching made him feel even more so. I was the only person who knew, and he had no intention of letting anyone else find out. I did my best to tell him that stuff like this happens to millions of other people, and that a doctor might be able to help him out. After doing some research on my own, I encouraged him even more to go to the doctor, since it might be eczema or psoriasis.
I wish Mick’s story ended there. But as I’m sure has happened to countless other cases, Mick ended up on a tour of all the doctors in his city and didn’t receive a diagnosis until visiting the second dermatologist that he found. The dermatologist prescribed steroid cream to manage the dry, cracking rashes. The creams each only worked for two months or so before they became ineffective. In reality, Mick couldn’t understand his disease until he visited a rheumatologist. Since then, working in the medical field, I’ve met many people with psoriasis, psoriatic arthritis and similar diseases who have gone through a similarly difficult process. If you have any of these symptoms, make sure to speak up to your doctor, or if you haven’t been able to find a doctor to help you, try some of the tips below.
I wrote this article using real clinical research, feel free to look at it yourself, the links are in the citations.
Types of Psoriasis
Psoriasis comes in many forms, multiple may be present at once, or just one may affect you. Psoriasis, while associated with your skin, is an inflammatory condition which can affect all sorts of tissues (Myers et al., 2020). If you already have one type of psoriasis, unfortunately others may follow.
Plaque Psoriasis is by far the most popular form of psoriasis, often appears after 20, and is the type that affected Mick. 90% of Psoriasis cases fit into this category, and it’s generally easy to identify. Red rashes appear that are raised from the skin and develop a rough, scaly texture, and even a silvery covering, sometimes called “wax spot phenomenon”. The rashes may appear in large or small blotches (Sarac et al., 2016). The affected areas aren’t gradually raised like mosquito bites however, they’re sharp edged and easily discernible. Most types of psoriasis share huge commonalities with plaque psoriasis.

Guttate Psoriasis is similar, however it appears as little spots which can be clumped or spread all over the body, these little bumps can grow to be considered plaques. Usually guttate Psoriasis affects small children, but can affect anyone, and is associated with changes in a test called the antistreptolycin titer. Make sure to ask your doctor or dermatologist if you believe you, your child, or a relative might have psoriasis.

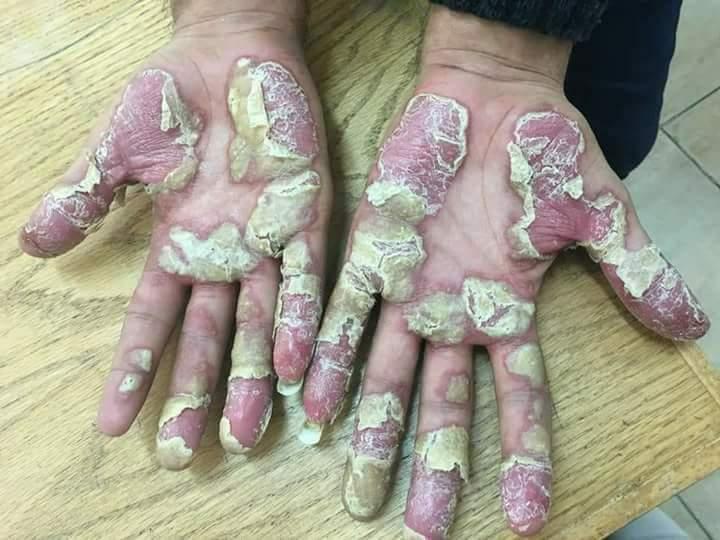
Palmoplantar Psoriasis affects the palms of the hands and soles of the feet. While rare (3-4% of psoriasis cases), this variant significantly affects hand/foot function, and can make daily activities difficult or painful. Here, the defining characteristic is the red rashes, which may be an extension of another form of psoriasis, or white formations, known as pustules (Palmoplantar pustulosis) on the thick padded region near the wrist, or towards the back of the foot. Deep cracks with possible bleeding could also occur here, making treatment all the more urgent. Pustulosis usually only appears in the ages from 20-60, and affects women four times as much as men (Miceli, Schmeider, 2020).
Inverse Psoriasis involves the red raised rash, but not the white growths which generally appear on plaque psoriasis. It forms on the folds of the skin and joints.
Erythrodermic Psoriasis is the most dangerous of psoriatic conditions. It is rare, only 1-2 percent of psoriasis patients develop Erythrodermic psoriasis. Like plaque psoriasis, a raised red rash is the defining characteristic, although in this case, the rash covers upwards of 60% of the affected person’s body. Since so much of the skin is affected complications are likely, such as edema of the lower limbs, organ failure, and hair loss, treatment must be found quickly to monitor for concerning features, as the risk of large scale infection is elevated (Singh et al., 2016).
Psoriatic Arthritis affects the joints, and causes joint pain and inflammation, which can even include the back. Less commonly, swollen fingers, eyes, and feet can also occur. This is one of the more painful conditions associated with psoriasis. Generally it is difficult to differentiate from Rheumatoid Arthritis (RA), although Psoriatic Arthritis doesn’t involve many of the classic RA symptoms, such as symmetric joint pain, dry mouth, and fatigue. Depending on the severity of the preexisting psoriasis, PsA can be up to 30% likely to manifest; it can also occur independently (Johnson, 2018).
In one form or another, there are over 100 million people with one or multiple forms of psoriasis, so you’re definitely not alone if you have it. For more info on prevalence, check out the National Psoriasis Foundation’s stats page. If you’re new to it, like Mick, and it seems like “normal” is a thing of the past, know that although there’s no cure, it is treatable to the level where most people can live the lives they want. When really well managed, psoriasis can go years without a flare-up.
Psoriasis generally occurs in the form of flare-ups. With existing psoriasis the rashes, spots, or inflammation may just worsen or appear larger in size and number. Although Psoriasis might seem like it just appears out of the blue, there’s two things that determine when the first flare-up appears. Your genetics are part of it, psoriasis runs in families and when it comes up, flare-ups are initiated by a trigger, which can be one of many things:
- STRESS – by far the biggest trigger
- Smoking tobacco
- Heavy drinking
- Infections, particularly large ones
- Cold and dry weather, the type that irritates skin
- Skin injury, including bites, cuts, and burns
- Some medications – Beta blockers, lithium, anti-malaria medication
- Rapid steroid withdrawals
- Obesity is considered a risk factor
If psoriasis in any form is already a part of your life, then avoiding, or learning to manage these factors can help you avoid flare-ups in the future. Fortunately, psoriasis is not contagious whatsoever. Psoriasis is bothersome, and at its worst it can affect your overall physical and mental health, but with good maintenance flare-ups can be avoided for months up to years. This is why it’s so important to have a healthcare provider familiar with psoriasis to help you find the right treatment for you. Scroll down for tips on finding a healthcare provider.
How it Works
When you can see the red blotches on your skin it’s easy to say that psoriasis is a skin disease. In reality however, it is an autoimmune disorder. This means that the immune system that was designed to protect you is actually acting against you in this case. Generally some event occurs which causes immune activation or simply the immune starts recognizing some innate proteins in your skin as unacceptable, and your immune system starts a response with the chemical messenger “Interleukin-17” which triggers a whole cascade of inflammatory mechanisms. Interestingly enough, this is the same inflammation pathway that causes Irritable Bowel Syndrome symptoms. IBS happens frequently with psoriasis, and that’s no coincidence (Zohar et al., 2016).
It’s not unusual for autoimmune diseases to operate through this inflammatory pathway. This shared feature might suggest an insight towards the right lifestyle to avoid treatment. Since a hefty fraction of the immune system of is connected to the intestine, a lifestyle/diet based approach could be the key to bringing your psoriasis under control. It could at least help. In psoriasis patients, studies have found that the gut microbiota (the population bacteria in your intestines, there’s trillions) is unbalanced, this means that the ratios of certain types of bacteria, are all out of whack, and the most important part is that biodiversity in your gut microbiome is reduced altogether. The gut microbiome has a large influence of the immune system, which suggests that a probiotic or diet based approach is feasible (Myers et al., 2020). There is research in this area, however there’s not enough hard evidence to devise a treatment based on these findings.
To put it short, it’s your immune system, not your skin that’s acting up.
Certain foods can actually increase inflammation in your immune system, such as red meat, salt, and fried foods. There are also plenty of foods which reduce it :), these could actually be a great benefit in some cases.
Now although this won’t cure your psoriasis, an anti-inflammatory diet can help soothe the intensity of your symptoms and reduce the likelihood of complications. The National Psoriasis Foundation has a page linking to more diet education here. This resource also has access to personalized help for your case also. If you’re already familiar with the topic, feel free to try these recipes.
Finding Treatment
Like Mick’s story above, finding a doctor which will give you the treatment you need can be exhausting. Don’t be dismayed by his process however, although he switches drugs plenty of times, most people with psoriasis only switch drugs about once a year. Here my goal isn’t to educate about the treatment, but to offer help on finding the right treatment provider. If you’re interested in learning more about psoriasis treatments themselves, Healthgrades has a great overview on them. Not everyone reacts the same to treatments, and no two cases are exactly alike, so don’t get used to using others’ treatments, progress, and severity as benchmarks for your own. With the right doctor, your individual case can be managed your individual way.
Primary Care Providers are usually the first stop with any illness. Your insurance might also require that you visit your Primary Care Doctor before you visit any specialist anyways, and they typically have a good understanding of 90% of the diseases under the sun. A good Primary Care Doctor who has seen a lot of psoriasis cases could help you get started on your psoriasis management journey by starting you on your first medication or by referring to a specialist that he personally recommends for psoriasis.
Dermatologists are the standard for psoriasis care. Although it primarily affects the skin, not all dermatologists might have a good understanding of psoriasis or many psoriasis cases in their clinic. To avoid doing all the loops that Mick went through, call ahead and ask if the office sees many psoriasis patients, or if psoriasis is one of their specialties. By finding a doctor who said yes to those questions, you’ve already saved yourself days or weeks of searching and hundreds of dollars as well, depending on how you pay. Before you visit, make sure you’re familiar with every aspect of your psoriasis: what aggravates it, when it started, when it goes away, etc… For more info check this page by the NPA.
Rheumatologists generally deal with autoimmune diseases that affect the joint and muscles, like rheumatoid arthritis and lupus. For this reason a rheumatologist can offer the best education and specialized treatment plan for Psoriatic Arthritis. To find the best rheumatologist for you, getting a referral from the dermatologist that you are seeing for psoriasis is a great place to start. Otherwise you can call ahead and inquire about psoriasis to get an idea of their level of familiarity. This site is a great resource for all about rheumatologists and psoriatic arthritis.
The psoriasis community is worldwide, nationwide, and has plenty of individuals in your community too. Connecting with individuals with the same frustrations can surely help finding the right doctors and courses of treatment. Online social media groups are easy to find and join. Besides the ones on the big social media platforms, there’s actually a dedicated platform for psoriasis, which makes it simple to share stories and advice, called MyPsoriasisTeam, which could be well worth checking out.
Final Thoughts
Psoriasis is not a small problem, but it is not impossible to manage. The most important things you or your friends and relatives suffering from psoriasis can do is to find the right care, and use your ability to self-educate to learn as much about your psoriasis as possible. Finding the right connections near you can also be a huge help in getting pointed in the right direction, so feel encouraged to reach out however you can. Successful management won’t be easy at first, but it can be easier with the right help.
Resources
“6 Must-Know Facts About Psoriasis – Sharecare.” Accessed July 14, 2021. https://www.sharecare.com/health/psoriasis-skin/article/must-know-facts-psoriasis?cbr=GGLE1500656&gclid=CjwKCAjw87SHBhBiEiwAukSeUXFlo0TdkH7y6FgTDphvX1qDcQHFUGcr-b36RcxmpFFSeSFC6bu90hoCp3wQAvD_BwE.
“Discovery of the IL-23/IL-17 Signaling Pathway and the Treatment of Psoriasis | The Journal of Immunology.” Accessed July 14, 2021. https://www.jimmunol.org/content/201/6/1605.
“I Tried An Anti-Psoriasis Diet. Here’s What Happened | Everyday Health.” Accessed July 14, 2021. https://www.everydayhealth.com/columns/health-answers/i-tried-an-anti-psoriasis-diet-heres-what-happened/.
Miceli, Alyssa, and George J. Schmieder. “Palmoplantar Psoriasis.” In StatPearls. Treasure Island (FL): StatPearls Publishing, 2021. http://www.ncbi.nlm.nih.gov/books/NBK448142/.
Myers, Bridget, Nicholas Brownstone, Vidhatha Reddy, Stephanie Chan, Quinn Thibodeaux, Alexa Truong, Tina Bhutani, Hsin-Wen Chang, and Wilson Liao. “The Gut Microbiome in Psoriasis and Psoriatic Arthritis.” Best Practice & Research. Clinical Rheumatology 33, no. 6 (December 2019): 101494. https://doi.org/10.1016/j.berh.2020.101494.
“Psoriasis – Symptoms and Causes – Mayo Clinic.” Accessed July 14, 2021. https://www.mayoclinic.org/diseases-conditions/psoriasis/symptoms-causes/syc-20355840.
Johnson, Jon. “Psoriatic vs. Rheumatoid Arthritis: What Is the Difference between Th,” May 24, 2018. https://www.medicalnewstoday.com/articles/321908.
Sarac, Gulbahar, Tuba Tulay Koca, and Tolga Baglan. “A Brief Summary of Clinical Types of Psoriasis.” Northern Clinics of Istanbul 3, no. 1 (June 14, 2016): 79–82. https://doi.org/10.14744/nci.2016.16023.
Singh, Rasnik K, Kristina M Lee, Derya Ucmak, Merrick Brodsky, Zaza Atanelov, Benjamin Farahnik, Michael Abrouk, Mio Nakamura, Tian Hao Zhu, and Wilson Liao. “Erythrodermic Psoriasis: Pathophysiology and Current Treatment Perspectives.” Psoriasis (Auckland, N.Z.) 6 (July 20, 2016): 93–104. https://doi.org/10.2147/PTT.S101232.
Zohar, Ariel, Arnon Dov Cohen, Haim Bitterman, Ilan Feldhamer, Sari Greenberg-Dotan, Idit Lavi, Doron Comanesther, Erez Batat, and Devy Zisman. “Gastrointestinal Comorbidities in Patients with Psoriatic Arthritis.” Clinical Rheumatology 35, no. 11 (November 2016): 2679–84. https://doi.org/10.1007/s10067-016-3374-y.